As you take a deep breath, have you ever wondered what’s happening inside your body? More specifically, what’s going on with the carbon dioxide (CO2) levels in your blood?
What is a Normal Blood CO2 Range?
In this blog post, we’ll dive into the world of hematology and explore what constitutes a normal blood CO2 range. But before we get started, let’s set the stage.
The Importance of Blood CO2 Levels
Blood CO2 levels play a crucial role in regulating various bodily functions, from breathing to energy production. When CO2 builds up in your bloodstream, it can lead to respiratory acidosis – a condition where your body produces more acidic blood due to excessive CO2 levels. On the flip side, low CO2 levels can cause respiratory alkalosis – a condition characterized by too much alkalinity in your blood.
Now, you might wonder why this matters. Well, understanding normal blood CO2 ranges is essential for diagnosing and managing various health conditions, such as sleep apnea, chronic obstructive pulmonary disease (COPD), and even neurological disorders like epilepsy. In the next section, we’ll explore the average range of blood CO2 levels in healthy individuals.
In our previous section, we explored the importance of blood CO2 levels in regulating various bodily functions. Now, let’s dive into the average range of blood CO2 levels in healthy individuals.
Normal Blood CO2 Range: What’s Considered Healthy?
A normal blood CO2 range typically falls between 22-26 mmHg (millimeters of mercury). This range is based on the American Thoracic Society’ guidelines and is considered a benchmark for healthy adults. However, it’s essential to note that this range may vary slightly depending on factors such as age, sex, and individual health status.
For example, newborns have a higher normal blood CO2 range of 25-30 mmHg due to their immature respiratory system. Similarly, elderly individuals may have a lower normal blood CO2 range due to changes in their respiratory function.
Factors Affecting Blood CO2 Levels
Blood CO2 levels can be influenced by various factors, including:
Respiratory rate: Faster breathing rates can increase CO2 levels, while slower rates may decrease them.
Cardiovascular function: Changes in cardiac output or peripheral resistance can affect blood CO2 levels.
Hormonal fluctuations: Hormone imbalances, such as those experienced during pregnancy or menopause, can impact CO2 levels.
Metabolic rate: Higher metabolic rates can increase CO2 production and lead to higher blood levels.
Understanding these factors is crucial for accurately interpreting blood CO2 levels and making informed decisions about patient care. For instance, if a patient has a high respiratory rate due to anxiety or stress, their blood CO2 level may be elevated even if their underlying condition is not related to respiratory issues.
Monitoring Blood CO2 Levels
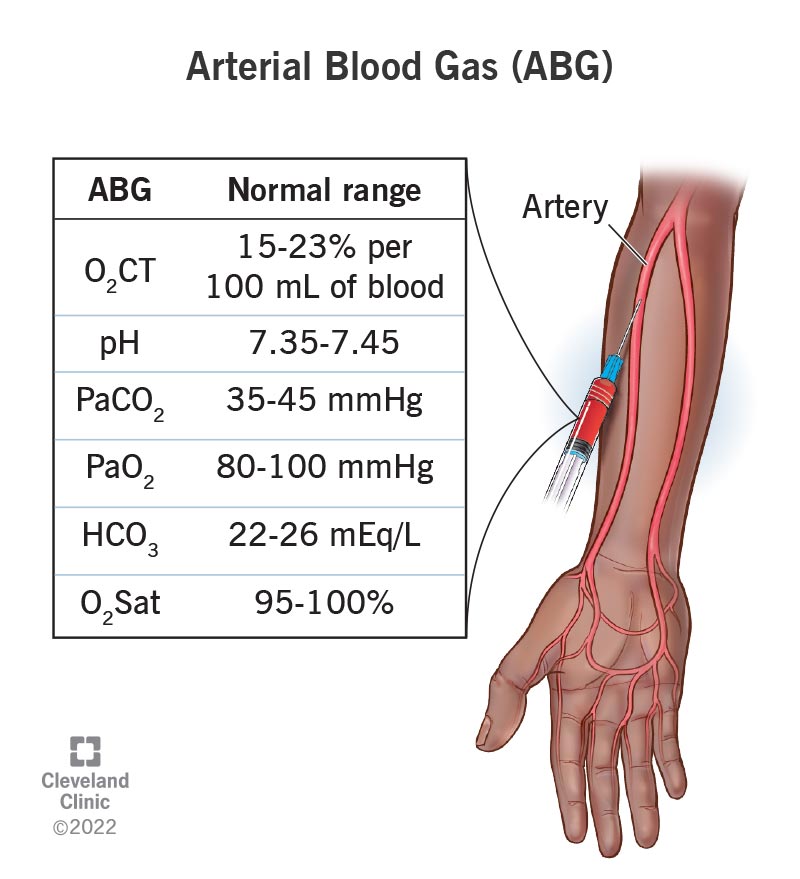
Blood CO2 levels are typically measured using an arterial blood gas (ABG) test. This non-invasive procedure involves collecting a small sample of blood from an artery, usually in the wrist or ankle. The ABG test provides valuable information about oxygen and carbon dioxide levels in your blood, allowing healthcare professionals to diagnose and manage various conditions.
It’s worth noting that there are also more advanced methods for monitoring blood CO2 levels, such as end-tidal CO2 (ETCO2) monitoring. This method uses a device placed on the patient’s nose or mouth to measure the CO2 content in their expired breath. ETCO2 monitoring is commonly used during anesthesia and critical care situations.
In our next section, we’ll explore common health conditions associated with abnormal blood CO2 levels and discuss the importance of proper diagnosis and management.
Get Expert Advice on Blood CO2 Levels
Speak with a medical expert to better understand your blood test results.
Consult a Medical ExpertIn our previous sections, we’ve explored the importance of blood CO2 levels and set the stage for understanding what constitutes a normal blood CO2 range.
Summarizing Our Key Points
We’ve covered how blood CO2 levels play a crucial role in regulating various bodily functions, including breathing and energy production. We’ve also discussed how abnormal CO2 levels can lead to respiratory acidosis or alkalosis, which can have significant implications for overall health.
Now that we’ve set the stage, let’s summarize our key points:
- Blood CO2 levels are essential for regulating bodily functions
- Abnormal CO2 levels can lead to respiratory acidosis or alkalosis
- A normal blood CO2 range is crucial for diagnosing and managing various health conditions
Final Insights
In conclusion, understanding the normal blood CO2 range is vital for maintaining overall health. By keeping an eye on your CO2 levels, you can identify potential issues before they become serious complications.
If you’re concerned about your blood CO2 levels or have questions about how to maintain a healthy range, consult with a healthcare professional today!
A Strong Conclusion
As we close this blog post, remember that the world of hematology is full of fascinating insights and practical applications. By embracing knowledge about normal blood CO2 ranges, you’re taking the first step towards a healthier, happier you.
Stay informed, stay empowered – and always keep breathing!
Star interview questions for customer service: Questions and best answers: Want to ace your next customer service job interview? Learn the top interview questions asked by hiring managers, along with expert tips on how to answer them like a pro.
Non-itchy rash on back and chest: What’s causing that pesky non-itchy rash on your back and chest? Get the lowdown on common causes, from allergic reactions to skin conditions, and find out how to treat it effectively.