As a pediatrician, you’re no stranger to navigating the complexities of your young patients’ health. One crucial aspect of their overall well-being is maintaining a healthy anion gap – a measurement that can reveal valuable insights into their metabolic status. But what exactly is this “anion gap” and why should you care about its normal range in pediatrics?
An Introduction to Anion Gap: Why It Matters in Pediatrics
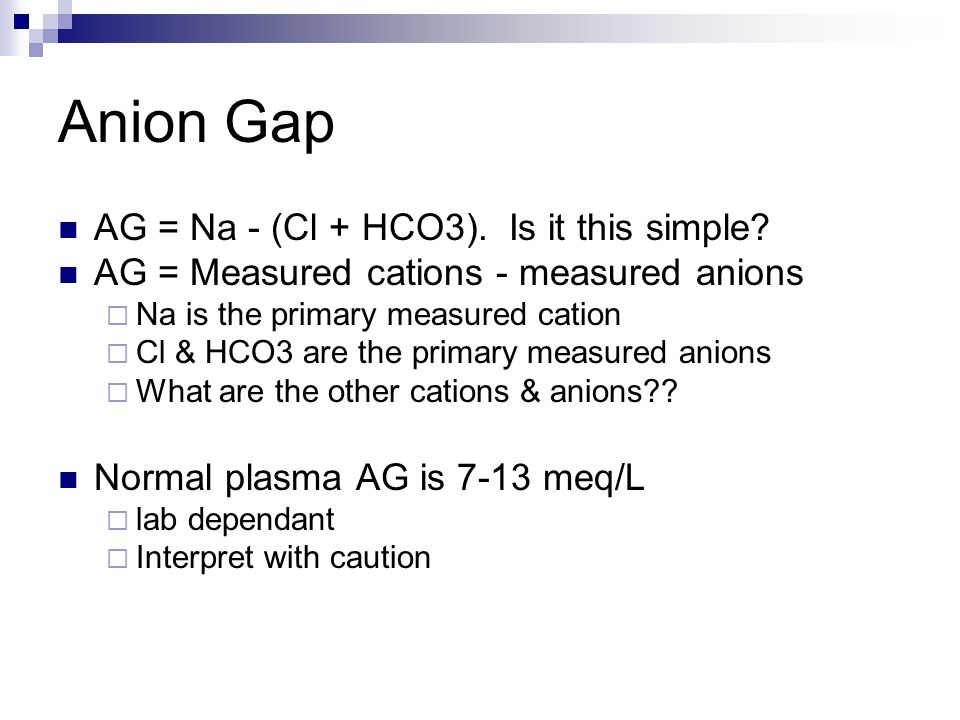
The anion gap, or AG, is a simple yet powerful tool that helps clinicians like yourself diagnose and manage various pediatric conditions. In essence, it’s the difference between the positively charged cations (like sodium) and the negatively charged anions (like chloride and bicarbonate) present in a patient’s blood.
The Importance of Anion Gap in Pediatrics
In pediatrics, maintaining a normal anion gap is crucial for ensuring proper metabolic function. A widened anion gap can signal underlying conditions such as diabetic ketoacidosis, sepsis, or lactic acidosis – all of which require prompt attention to prevent serious complications.
Anion Gap Normal Range in Pediatric Patients: What You Need to Know
So, what is the normal anion gap range for pediatric patients? In this first section, we’ll explore the answer and provide essential context to help you better understand its significance in your daily practice. Stay tuned for Part 2, where we’ll dive deeper into the clinical implications of an abnormal anion gap in pediatrics.
In our previous section, we introduced you to the concept of anion gap and its importance in pediatrics. Now, let’s dive deeper into the normal range for pediatric patients.
Anion Gap Normal Range in Pediatric Patients: What You Need to Know
The normal anion gap range for pediatric patients varies depending on age group. For newborns (less than 28 days old), the normal range is typically around 3-8 mmol/L. In infants and toddlers (28 days to 2 years old), the range is slightly wider, ranging from 4-12 mmol/L. For older children (2-18 years old), the normal anion gap range is generally narrower, falling between 5-10 mmol/L.
It’s essential to note that these ranges are general guidelines and may vary depending on the specific laboratory methods used to calculate the anion gap. Factors such as electrolyte imbalances, kidney function, and medication use can also influence the anion gap result.
What Causes an Abnormal Anion Gap?
An abnormal anion gap can indicate a range of underlying conditions, including:
- Diabetic ketoacidosis, which requires prompt attention and management.
- Sepsis or systemic infections, which can lead to metabolic acidosis if left untreated.
- Lactic acidosis, often seen in patients with severe sepsis, cardiogenic shock, or other high-energy demands.
In the next section, we’ll explore the clinical implications of an abnormal anion gap in pediatrics, including diagnosis and management strategies. Stay tuned for Part 2!
Consult with Pediatric Experts
Get expert advice on anion gap normal range in pediatric patients. Our team of medical professionals is here to help.
Schedule ConsultationIn conclusion, understanding the normal range of anion gap in pediatric patients is vital for diagnosing and managing various conditions that can impact their overall health. As a pediatrician, it’s essential to be aware of this critical measurement and its implications on your young patients’ metabolic status.
By recognizing the importance of maintaining a healthy anion gap, you’ll be better equipped to identify potential issues early on, allowing for timely interventions and improved outcomes. Remember, a widened anion gap can signal more serious conditions that require prompt attention – so stay vigilant and stay informed!
A Final Word: The Power of Anion Gap in Pediatric Practice
As you continue to care for your pediatric patients, keep the anion gap in mind as a valuable tool for uncovering underlying metabolic issues. By incorporating this measurement into your daily practice, you’ll be empowering yourself with a powerful diagnostic and management strategy that can make all the difference in the lives of your young patients.
Join us next time for Part 2 of our series on anion gap in pediatrics, where we’ll delve deeper into the clinical implications of an abnormal anion gap and explore practical tips for incorporating this measurement into your practice. Until then, stay informed, stay vigilant, and keep those pediatric patients healthy and thriving!